- What is a cataract?
- What causes cataracts? How does one get them?
- What are the symptoms of cataracts?
- Do I have to wait for my cataracts to "ripen"?
- What are my options for treatment?
- What are the different types of IOLs? Are there differences in quality?
- What are the preparations before cataract surgery?
- What is the recovery time after surgery? Any physical limitations?
- Will I still wear glasses after cataract surgery?
- Do I need to come back after surgery?
- What are the complications of cataract surgery?
- Do cataracts come back after surgery?
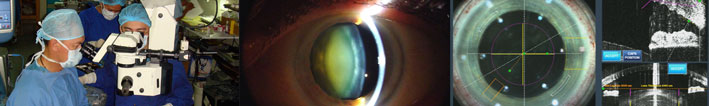
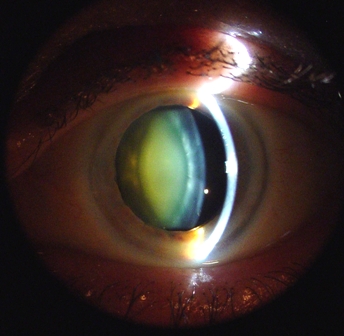
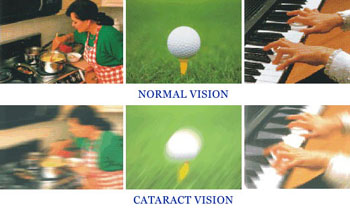
The transparent human lens, like the lens of a camera, focuses light rays onto the retina (the camera "film"). A cataract is any opacity in the lens that interferes with light transmission through the eye resulting in decreased visual function. Clinically, this is manifested as "blurred vision", "cloudiness of vision", "poor night vision", or "glare."
What causes cataracts? How does one get them?
Most cataracts develop as part of the aging process. It is probably safe to say that anyone who lives long enough will eventually develop cataracts. The pace of cataract development varies from individual to individual and is influenced by environmental factors (e.g. long term exposure to ultraviolet or UV rays seen more in tropical countries). Since countries closer to the equator have greater UV exposures (like the Philippines), cataracts here tend to be thicker and harder compared to those seen in temperate countries. Other causes of cataract include medical conditions like diabetes, or intake of certain drugs like steroids. There are also congenital and juvenile cataracts. Infections, inflammations and injuries can likewise cause cataracts.
What are the symptoms of cataracts?
In addition to painless blurring of vision, patients complain of cloudy vision, poor night vision, glare, light sensitivity, and a yellowish discoloration or drabness of colors.

In some patients, the progression of the cataractous lens acts like a "reading lens" and may temporarily give some patients better near vision, a phenomenon called "second sight". This "improvement in vision" of course, is only temporary as the vision later worsens with further cataract progression. When this occurs, persons with cataract will have worsening symptoms negatively affecting even activities of daily living.
Do I have to wait for my cataracts to "ripen"?
A product of the old-school, one of the persistent myths about cataract surgery nowadays is that one needs to wait for a cataract to "ripen". Different people have different visual needs depending on their profession and way of life. Once the cataract (even in its early stages) is significant enough to interfere with one's activities, then one should consider cataract surgery. One that utilizes the latest equipment and techniques, and is performed by experts in the field to guarantee success.
The American Eye Center (AEC) has always been the leader in providing its patients with the most modern cataract surgery technique that allow for almost instantaneous visual recovery and minimal "down time" before resumption of personal and even profession-related activities. AEC's treatment goal is to provide individuals with vision they once enjoyed during their youth and to eliminate, in varying degrees according to the patient's choice, the need for spectacles after cataract surgery. All this, within the shortest time and with the least discomfort and risk. AEC's unequaled population of happy patients is testament to it's success in providing only the best.
What are my options for treatment?
The Old Ways:
Although so-called "anti-cataract" eyedrops from reputable pharmaceutical companies are available in drugstores (including herbal remedies or "cleansing diets" for cataract treatment), there is still no convincing evidence that medical therapy works in reversing the process of cataract progression. The only scientifically proven method of treating cataracts is still surgery.
Until recently, cataract surgery involved a very large incision in the globe to remove the lens in toto (intracapsular cataract extraction or ICCE), or leaving the posterior capsule behind to support an intraocular lens or IOL (extracapsular cataract extraction or ECCE). Both techniques require several sutures to close the wound, and are performed under general anesthesia or retrobulbar anesthesia (anesthesia injection behind the globe), taking anywhere from 30 minutes to an hour to perform. In ICCE, hardly performed in developed countries today, patients need to wear very thick glasses after surgery to compensate for the natural lens that was removed. Although more advanced than ICCE because an intraocular lens or IOL can be implanted inside the eye, ECCE still has major disadvantages associated with a large wound. In spite of these disadvantages, many ophthalmologists in the country today still perform cataract surgery via ECCE.
Modern-day Cataract Surgery:
Phacoemulsification
State-of-the-art cataract surgery involves a very small incision (less than 1/8th of an inch) in the cornea wherein a probe is inserted with the purpose of breaking up the cataract and removing the pieces by aspiration. This procedure is called phacoemulsification and is more familiar to the lay person as "no-stitch" or "stitch-less" surgery. AEC surgeons not only were the pioneers in this type of surgery in the Philippines but continue to remain in the forefront in it's innovation, improvement and instruction both nationally and internationally. The American Eye Center likewise settles for nothing less than the best and latest in technology using the remarkable Alcon Infiniti Vision System. As the small incision in phacoemulsification is self-sealing, no sutures are needed. A relatively recent technological advancement, the "foldable" IOL" (see discussions below) is inserted through this incision, preserving the small size and self-sealing nature of the wound. The whole process is done under "eyedrop anesthesia" and is usually completed in 15 minutes or less. Because of the elimination of the need for general or injection anesthesia, the absence of bleeding and eye covers ("patching"), and the almost instantaneous (within hours after surgery) return of good visual function even without glasses, phacoemulsification is commonly but erroneously referred to as "laser eye surgery." While this procedure is currently the standard for cataract removal worldwide, it is NOT laser cataract surgery. True laser removal of cataracts was previously unavailable to patients, until very recently (see next section on femtosecond cataract surgery). Phacoemulsification is routinely performed at the American Eye Center and is available as a surgical option for our patients with cataracts.
Femtosecond Cataract Surgery:
A new treatment for cataracts was recently unveiled at the American Eye Center that promises to provide patients with the most advanced all-laser cataract procedure---the first of its kind in Asia. Dubbed the Alcon LenSx femtosecond laser surgery, this new equipment brings an unprecedented level of safety, speed and precision in treating cataracts, and enhances the host of options for surgical-based methods that AEC offers its clients.
The Alcon LenSX femtosecond laser differs from the traditional methods of cataract surgery by the absence of the blade. By using very short yet intense bursts of near-infrared light, the Alcon LenSX femtosecond laser technology is able to create extremely precise subsurface cuts without manual intervention The blades used to create the small incisions in the eye have been completely replaced by this laser, making the incisions more precise and predictable. In addition, the circular opening that is created in the human lens in order to access the cataract (called a capsulotomy) which was traditionally performed by human hands has now been replaced by the femtosecond laser, making the capsulotomies more architecturally round and centered. Studies have shown that this is very important in intraocular lens stability and refractive predictability of surgical outcomes (In one study by the American Academy of Ophthalmology, femtosecond laser incisions achieved perfect capsulotomy diameter accuracy in 100 percent of cases). Finally, the actual cataract is also fragmented by the femtosecond laser making it much easier and less traumatic for the surgeon to remove and clean it up prior to placement of the IOL. In short, the femtosecond laser has replaced many of the steps in the cataract surgery that were previously performed by human hands, i.e., resulting in less surgical error and better predictability of outcomes. Results are more precise than any other previous or current methods of cataract surgery.
The Alcon Lensx Laser system is currently available ONLY at the American Eye Center. Arguably the most advanced method for cataract surgery today, it is now readily available in our center as one of the surgical options for cataract surgery. (www.lensxlasers.com)
Will I still wear glasses after cataract surgery?



The Role of Intraocular Lenses (IOLs)
Before the advent of IOLs, patients undergoing cataract surgery had no choice but to wear very thick glasses to compensate for the natural lens that was removed during surgery. Not only were they unsightly but, more importantly, these gave wearers extremely magnified images and limited fields of vision that were far from normal.
Since the advent of IOLs sometime in the middle of the last century, it is now possible for patients to recover the quality of vision they enjoyed prior to the onset of their cataracts. In fact, for those who had to use spectacles to achieve normal vision, it would even be better because the IOL can eliminate, or at least limit, their dependence on glasses.
The American Eye Center doctors and other qualified staff will discuss the varied options for visual rehabilitation with patients beforehand with the end objective of providing vision that the patients will be happy with after surgery. To achieve this, several levels of spectacle independence can be targeted. First is the freedom from having to wear glasses for distance vision. If this is the patient's choice, an IOL will be implanted which will give the patient good spectacle-free vision for distance. However, glasses will be necessary for near work (reading and computer). The second option is one wherein the patient prefers to be able to read without glasses and won't mind spectacle wear to be able to see well for distance. The third, and most attractive for the majority, is not having to wear glasses at all for the full range of vision (distance, computer and reading).
What are different types of IOLs? Are there differences in quality?
In recent years, significant advances in IOL technology has made it possible to manage cataracts like a refractive procedure. Nowadays, patients can have superior quality vision after their surgery without having to wear glasses. This is possible with the implantation of intraocular lenses or IOLs.
There are three major categories or types of intraocular lenses in cataract surgery. Each type determines the kind of vision (good distance, good reading, or both) that the patient will have after surgery. The first type is the monofocal IOL. This lens has only one grade which is chosen for the patient through biometry (please see discussion on preparations before surgery) usually to give him/her good distance vision without having to wear eyeglasses. The second type is the monofocal toric IOL. This lens is recommended for those who have astigmatism which needs to be corrected in order to achieve spectacle independence for distance. In both these types, patients will require glasses for near work (reading and computers). The third category is what is called the "presbyopia-correcting IOLs." These lenses make it possible to have spectacle independence in at least 90% of the patient's visual requirements (distance, computer and reading). Multifocal and accommodating IOLs are the two types of presbyopia-correcting lenses also come in astigmatism-correcting varieties.
There is a fourth type of intraocular lens which is called the phakic IOL (also known as an intraocular contact lens or ICL). This, however, is implanted in the eye with the normal non-cataractous natural lens still in place. These are used to correct high grades of myopia (nearsightedness) beyond the range of laser (LASIK) treatment.
American Eye Center surgeons are indisputably the leaders in advanced IOL technology. They have the largest experience in their use which translates to excellent results. The Center's experiences and results are often presented in both national as well as international meetings and are used as gauges of success by others worldwide.
"Not all IOLs are created equal." As in all consumer products, whether it be clothes, accessories, machines, gadgets, food, and others, there are differences in quality. The same is true for IOLs. Intraocular lens quality is determined by, among others, the material used, the design and structure, the smoothness of it's surface, and certain add-ons like filters against ultraviolet light and blue light. These features determine their long-term safety and stability in the eye. Another feature one looks at is the consistency and accuracy of the built-in grades of these IOLs. An important term that comes to mind is "quality control." When refractive results have to be as accurate as it should be in cataract surgery, eye surgeons have to be able to rely on IOLs that can deliver what they have on their labels. Unfortunately, not all IOLs have these. At the American Eye Center only the highest quality IOLs are used to ensure the best results possible.
The variety of IOLs, their advantages and limitations, and the desired target outcomes will be discussed in detail by the doctor at the American Eye Center to help the patient decide as to what best suits their lifestyle goals.
What are the preparations before cataract surgery?
A. Eye examination
A "basic" eye examination is conducted on the initial consultation of a patient with complaints that may be attributed to cataracts. An eye specialist (ophthalmologist) will then examine the patient and once it has been established that cataract is indeed the primary cause of the visual complaints, treatment options will be discussed. If the choice is cataract surgery, a more detailed work-up will ensue which will include, among others, a biometry. This is a measurement of the eye necessary to calculate the power of the intraocular lens (IOL) that will be implanted in the eye during the procedure. At the American Eye Center, this crucial test is performed with the technology's most advanced and most accurate machines which are the IOLMaster and the Lenstar.
B. Health status assessment
Generally, for patients over 40 years old and especially those with known heart, lung or other ailments, most ophthalmologists will require a cardio-pulmonary clearance either from the patient's personal physician or from one that the Center can recommend. Not all, however, are required to undergo this procedure and we encourage patients to discuss this with the eye doctor.
C. Immediate preoperative preparation
Pre-operative eyedrops are instilled in the eye 1-3 days before the scheduled surgery. Some oral medications being taken by patients for other health conditions may have to be discontinued several days to a week prior to surgery. Your internist and eye surgeon will advise you regarding this during the preoperative counseling and scheduling.
What is the recovery time after surgery? Any physical limitations?
In the past, patients had to stay overnight in a hospital for cataract surgery. Fortunately, modern day cataract surgery should not have to be that inconvenient and costly. The American Eye Center has a fully-equipped world class operating room suite that can rival the best surgical suites in advanced countries. The cataract surgery is performed on an out-patient or ambulatory basis.
In contrast to ICCE and ECCE, where patients had several physical limitations after surgery (limited coughing, sneezing, straining, bending over, etc.), patients undergoing phacoemulsification literally get up from the operating table immediately after surgery, change back to their street clothes, and are ready to go home in a few minutes with only a transparent eye shield as evidence of the surgery. Most patients already notice a significant improvement in vision a few hours after surgery, and it is expected to be 'optimal' by the next day. In some, this may take slightly longer depending on many factors which doctors discuss with each patient. Most regular, non-strenuous physical activities are resumed the next day. Though vision is good enough to drive a car the day after surgery, the performance of this activity, as well as other special activities will depend on one's confidence/capabilities. It is usually recommended that excessive water getting into the eye be avoided for 1-2 weeks to minimize the risk of infection. An eye shield to keep the eye from being pressed or rubbed during sleep is optional. Full recovery and the cessation of all limitations is generally achieved in three weeks time.
Do I need to come back after surgery?
As with any surgery, follow-up care is very important. One is usually asked to come back for follow-up one to two days after surgery, at one week, and then at one month after surgery. As there will be several eye drop medications that patients will be asked to apply to ensure optimum recovery, it will be necessary to monitor patients on a regular basis. By one month, full recovery would have been achieved.
What are the complications of cataract surgery?
As one of the most successful procedures performed today, cataract surgery should be more than 99% successful in a skilled surgeon's hands and in a reputable center. One should realize however, that blurred vision in the elderly does not always result from cataract alone, and may be the result of problems in the retina or optic nerve. In an otherwise "healthy" eye with cataract, successful cataract surgery should fully restore the vision without any problems. The risks of serious complications (such as bleeding, infection, corneal decomposition, macular edema, retinal detachment, etc.) are extremely rare, and individual statistics on these may be discussed with your doctor thoroughly.
Do cataracts come back after surgery?
Patients suspect recurrence of cataracts when their vision deteriorates from what was clear right after surgery.
Once removed, cataracts do not grow back or recur. What is almost always mistaken for this is what is called an "after-cataract" or posterior capsule opacification (PCO). This is due to either the formation of a thin fibrous tissue or the accumulation of cells behind the IOL or both causing blurred vision. All that is required to restore clear vision is a simple, out-patient, woundless and painless five minute laser procedure that creates a window through this tissue.