Diabetic Retinopathy
- What is diabetes?
- What is diabetic retinopathy?
- What are the stages of diabetic retinopathy?
- What are the symptoms of diabetic retinopathy?
- How is diabetic retinopathy detected?
- Who should get eye check-ups?
- What is the treatment for diabetic retinopathy?
- What can be done to prevent diabetic retinopathy?
- Can something be done if diabetic retinopathy is advanced and detected late?
Age Related Macular Degeneration
- What is macular degeneration?
- What are the symptoms of AMD?
- What are the types of macular degeneration?
- What causes AMD?
- What can be done for AMD?
- Can something be done if AMD is advanced and detected late?
Retina Screeening
- What is Retina Screening?
- How is dilation of the pupil done? What changes do you expect?
- What is the Retina?
- Why do you need retina screening?
- What are flashes and floaters?
- What is Posterior Vitreous Detachment?
- Retinal Detachment
- What can be done for a retinal break, hole or tear to prevent a retinal detachment?
- Is the Retina Screening done for other eye problems?
Diabetes mellitus is a chronic disease characterized by inability to utilize the sugars (carbohydrates) in our diet. It is caused by insufficient production of insulin by the pancreas. Uncontrolled diabetes frequently affects the eyes and can cause cataracts, glaucoma, optic nerve problems and most significantly damage to the blood vessels of the retina which results in diabetic retinopathy. Diabetes can affect adults and children as well.
What is diabetic retinopathy?
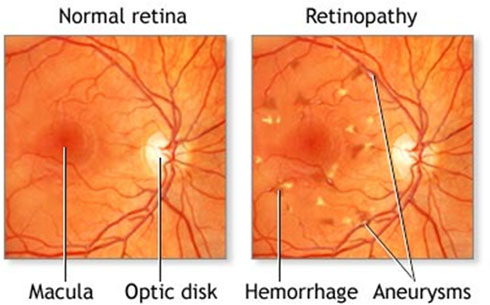
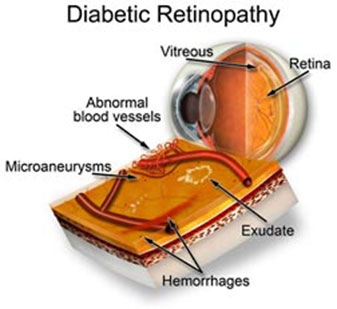
Diabetic retinopathy is a complication of diabetes mellitus that affects the inner part of the eye called the retina. The retina is the innermost lining of the eye and is responsible for receiving visual images for transmission to the brain.
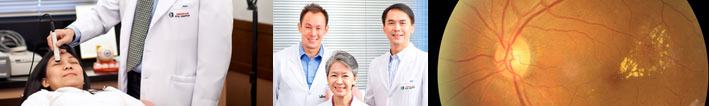
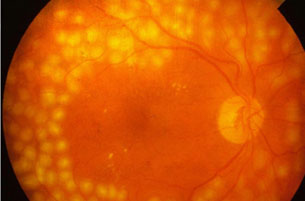
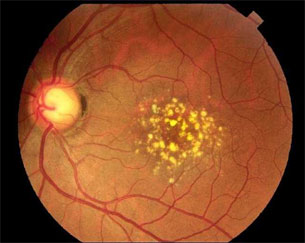
Diabetes causes changes in the blood vessels of the retina that leak fluid and/or blood. The smaller blood vessels called capillaries become narrowed and/or obstructed while others form balloon-like sacs. These changes cause the vessels to leak blood and fluid, seen as hemorrhages, exudates and/or swelling.
Diabetic retinopathy is also one of the leading causes of blindness, especially if undetected or left untreated.
The risk of developing diabetic retinopathy increases the longer the patient has diabetes and the poorer the sugar control is.

What are the stages of diabetic retinopathy?
There are two major stages of diabetic retinopathy: 1) Non-Proliferative Diabetic Retinopathy (NPDR) and 2) Proliferative Diabetic Retinopathy (PDR).
Nonproliferative Diabetic Retinopathy
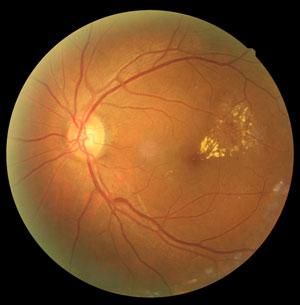
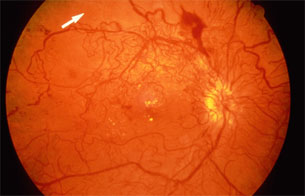
Non-proliferative diabetic retinopathy is manifested in the retina as red dots and blots of hemorrhages and/or as yellow dots which are actually lipid (fatty) leakages. If the macula (the central portion of the retina responsible for acute vision) is affected, significant blurring of vision that cannot be fully corrected with eyeglass prescriptions may be noticed by the patient.
These retinal changes increase both in size and severity the longer the patient has diabetes. The speed with which the retinopathy progresses will primarily be determined by the patient's level of sugar control.
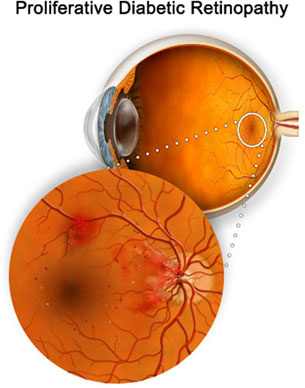
Proliferative Diabetic Retinopathy
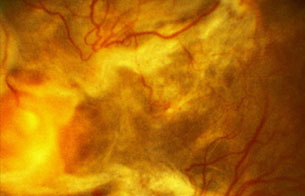
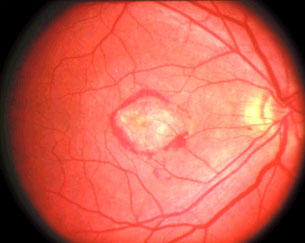
Proliferative diabetic retinopathy is the more advanced stage where abnormal new blood vessels begin to grow on the surface of the retina as a compensatory mechanism for the decreasing blood flow brought about by the capillary abnormalities. In the earlier stages of the proliferation, the blood vessels grow on the surface of the retina. Later, however, these blood vessels begin to extend upwards and grow into the fluid of the eye called the vitreous. Unfortunately, these new vessels are weaker and have a tendency to rupture and/or leak causing hemorrhage in the eye cavity which could result in severe blurring of vision or blindness. With the continued growth of the abnormal blood vessels on the retina, extensive bleeding and scar formation can likewise happen and cause severe sight threatening conditions such as traction retinal detachment.
What are the symptoms of diabetic retinopathy?
The most common symptom is gradual, continuous blurring of vision. This can be due to the swelling of the macula in the earlier stages. The blurring may be mild to quite severe depending on the seriousness of the retinopathy. In the proliferative diabetic retinopathy stage, the blurring may be sudden and severe due to the bleeding of the vessels into the cavity of the eye.
Many times, the patients can describe the start of the vitreous hemorrhage. In the beginning, they see black spots or dots called "floaters". These dots occasionally become elongated like strands of hair that eventually become denser and blacker. The vision then becomes quite poor as the blood increases and fills the vitreous.
Progression of the condition, including increase in hemorrhage and scar formation may threaten good vision and result to irreversible visual decline.



How is diabetic retinopathy detected?
To detect diabetic retinopathy, a comprehensive eye exam including a retina screening is performed by your eye doctor. A retina screening involves dilating the pupil in order to be able to see the retina adequately via specialized equipments.
If diabetic retinopathy is noted, color photographs and/or fluorescein angiography are recommended. Fluorescein angiography (FA) is a special technique performed which allows detailed analysis of the blood vessels of the retina and helps determine the seriousness of the retinopathy to plan for the mode of management. Optical coherence tomography (OCT) may also be recommended. This exam evaluates the thickness of the retina to give a better picture of the severity of the macular edema.
Who should get eye check-ups?
All diabetics should go for eye check-ups which include evaluation of the retina by a qualified retina specialist.
Type 1 diabetics should undergo a comprehensive eye exam including retinal screening 3-5 years after initial diagnosis. However, type 2 diabetics are recommended to undergo the same as soon as they are diagnosed.
Diabetics who become pregnant and those diagnosed with gestational diabetes should have retinal checks prior to conception and early in the 1st trimester, then every trimester thereafter or as recommended by the retina specialist.
What is the treatment for diabetic retinopathy?
Treatment depends on the stage of the retinopathy. If the retinopathy is still in the early nonproliferative diabetic retinopathy stage, repeated eye checks are recommended.
If the diabetic retinopathy is progressing, retinal photos and a fluorescein angiography (FA) may be requested to document the stage of the disease. This exam involves injecting a dye into the arm vein and taking photos of the retina to see which vessels are leaking or which areas lack adequate blood supply. Moreover, an FA may help decide if laser treatment for the retinopathy is needed and how soon the laser treatment should be started.
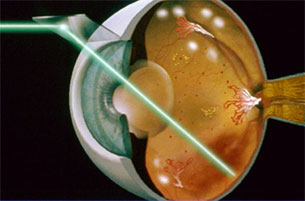
At the appropriate stage, PRP or pan-retinal photocoagulation (laser of the retina) is performed to prevent the blood vessels from growing continuously, thereby preventing bleeding. Most significantly, appropriate timing of PRP can prevent blindness.
If you are diagnosed as having diabetic macular edema, laser therapy of the macular portion or intraocular injections of medications may be recommended.
If cataracts are present, a cataract operation may be recommended.
If blood is noted in the vitreous or in more advanced cases where scar tissue has caused the retina to detach, a surgical procedure called pars plana vitrectomy may be recommended to repair the condition.

What can be done to prevent diabetic retinopathy?
Large scale studies have shown that prevention of Diabetic Retinopathy can primarily be achieved with a very tight control of blood sugar.
It is also very important that the patient comply with the schedule recommended by the retina doctor for follow up visits even if the patient does not feel any symptoms. This is because diabetic retinopathy will more often than not start quietly and the patient may experience symptoms only when the disease is in its more advanced stages.

Can something be done if diabetic retinopathy is advanced and detected late?
Yes. Vision rehabilitation can help you cope with changes in your vision so that you can continue to lead an independent and active life. Know more.
What is macular degeneration?
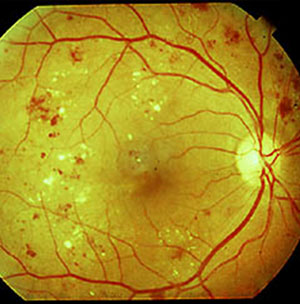
Macular degeneration or age related macular degeneration (ARMD/AMD) is a common cause of central vision loss in people over the age of 55. It is a progressive breakdown of the macula, the central portion of the light sensitive membrane at the back of the eye that can lead to loss of ability to read, drive or even recognize faces.
What are the symptoms of AMD?
AMD should be suspected in people over 55 years of age if they experience any of the following:
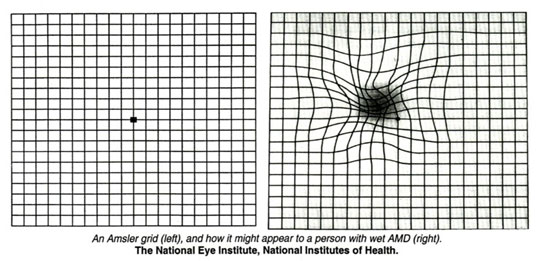
- distortion: straight lines appear wavy or bent
- difficulty reading, driving, recognizing faces or any tasks that require fine vision
- dark patches or "blind spots" in your central field of vision


What are the types of macular degeneration?
There are primarily 2 types of macular degeneration, the "dry" or atrophic type of AMD wherein the light sensitive cells of the retina degenerate and thins out; and the "wet" or neovascular type wherein abnormal blood vessels have grown into the central portion of the retina causing leakage of fluid, bleeding and sometimes scar formation.
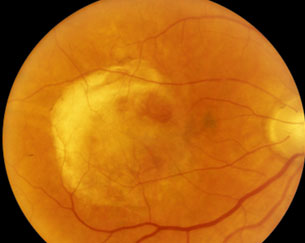
What causes AMD?
The cause of AMD is multifactorial. The central portion of the retina including its cells and supporting structures presumably undergoes oxidative stress causing it to break down and lose function. Age, hypertension and smoking are just some of the proven risk factors in the development of AMD. Thus, essential in the treatment of the ocular condition is also the control of all these systemic risk factors. Some other risk factors that are thought to be contributory include poor diet, increased exposure to UV rays, and light iris pigmentation.
What can be done for AMD?
The most important step in treating AMD is early recognition. If the disease is diagnosed early, a variety of treatment options is available to you. Regular annual eye examination with your ophthalmologist may reveal early lesions that would otherwise be asymptomatic. Should your ophthalmologist suspect AMD, ancillary procedures like fluorescein angiography (FA) and optical coherence tomography (OCT) may be requested to determine the extent of the lesion.
For "Dry" AMD, studies have shown that supplementation with pre-specified dose of vitamins A,C,E, Selenium and Zinc can help retard the progression in certain cases. Cessation and control of other risk factors are highly recommended.
For "Wet" AMD, a variety of treatment options are now available depending on the type and stage of the lesion, its size, location and accompanying findings. Laser photocoagulation, photodynamic therapy and intraocular injections of a variety of medicines can help retard or even reverse the process to a certain extent.
When seen at the correct time, laser treatment can be applied to seal the retina break/hole/tear and help prevent a retinal detachment. When detachment occurs, a procedure called vitrectomy may be performed to repair it. Because of this, it is highly recommended that retinal screening be done at regular intervals: 3, 6 or 12 months depending on the findings seen during screening. Findings may be acceptable now but can change in time.
Can something be done if AMD is advanced and detected late?
Yes. Vision rehabilitation can help you cope with changes in your vision so that you can continue to lead an independent and active life. Know more.
When seen at the correct time, laser treatment can be applied to seal the retina break/hole/tear and help prevent a retinal detachment. When detachment occurs, a procedure called vitrectomy may be performed to repair it. Because of this, it is highly recommended that retinal screening be done at regular intervals: 3, 6 or 12 months depending on the findings seen during screening. Findings may be acceptable now but can change in time.
What is Retina Screening?
Retina screening is the meticulous examination of the retina for any signs of weakness or other significant findings. To perform this exam it is better to dilate the pupil.
How is dilation of the pupil done? What changes do you expect?
Your pupils will be dilated with eyedrops instilled at 10-20 minute intervals for about 3 doses in general. There may be a slight stinging discomfort with each drop.
It may take as long as 20-60 minutes to achieve the needed effect and much longer if you are diabetic. In most patients, reading becomes difficult and that room light becomes glaring.
The effects of dilation may last as long as 4-6 hours after which, your vision goes back to how it was pre-dilation. It will be difficult to read and drive. Pupil dilation is needed to perform a more thorough exam of the retina.
What is the Retina?
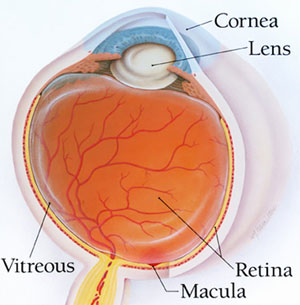
The retina is the very thin light-sensitive layer of tissue at the back of the inner segment of the eye. The eye is filled with vitreous- a substance as clear as water but gelatinous in consistency. Functionally, the retina acts like the film in a camera -- images come through the eye's lens and are focused on the retina. The retina then converts these images to electrical signals and sends them via the optic nerve to the brain. The retina is normally reddish in color due to its rich blood supply. An ophthalmoscope allows your ophthalmologist to see through your pupil and lens to the retina. If any changes in the color or appearance of the retina is observed, it may indicate a disease. Anyone who experiences changes in sharpness or color perception, flashes of lights, floaters, distortion in vision, or cuts in one's visual field, one should get a retinal examination.
Why do you need retina screening?
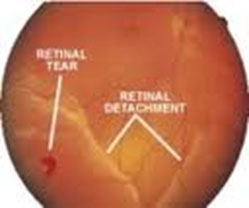
There are some conditions in the retina which, if seen at the appropriate time, can be treated to prevent a more severe problem. One of these is called a retinal break/tear/hole. This form of lesion can lead to a condition called Retinal Detachment where the retina becomes "peeled off" by fluid entering through the hole to go behind the retina- just like how the white meat of the coconut is scraped off its shell. If detected at an appropriate time, laser treatment of the retina (sealing of the hole to prevent entry of fluid) can be performed to prevent a detachment. Otherwise, major surgery is usually needed to fix a Retinal Detachment.
Myopia (nearsightedness) leads to a higher risk for developing these areas of weakness or retinal breaks/tears/holes. However, normal eyes can also have this problem at a much lower incidence. In most cases, patients will experience flashes of light and floaters before a Retinal Detachment develops.
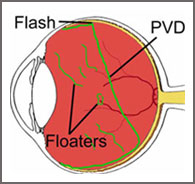
What are FLASHES AND FLOATERS?
Floaters
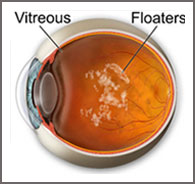
Eye floaters are those mosquito-like specks and "cobwebs" that drift aimlessly around in your field of vision. While annoying, these are very common and usually are not cause for alarm. These typically appear when tiny pieces of the eye's gel-like substance (vitreous) break loose within the hollow portion of the inner eye.
When we are born and throughout our youth, the vitreous has a gel-like consistency. But as we age (usually after 50 years of age but sooner in myopic eyes), the vitreous begins to dissolve and liquefy to create a watery center occurring over a span of months or even years. Some remaining formed gel particles occasionally will float around in the more liquid center of the vitreous. These particles can take on many shapes and sizes to become what we refer to as "floaters."
You'll notice that these floaters are particularly pronounced when you look at a bright, clear sky or a white computer screen. But you cannot see the actual tiny bits of debris floating loose within your eye. Instead, shadows from these floaters are cast on the retina as light passes through the eye, and those shadows are what you see. You'll also notice that most of these specks never seem to stay still when you try to focus on them. Floaters and spots move when your eye moves, creating the impression that they are "drifting."
Flashes
Ordinarily, light entering your eye stimulates the retina. This produces an electrical impulse, which the optic nerve transmits to the brain. The brain then interprets this impulse as light or some type of image. If the retina is mechanically stimulated (physically touched), a similar electrical impulse is sent to the brain. This impulse is then interpreted as a "flicker" of light. This happens in an age-related benign condition called posterior vitreous detachment (PVD). This does not lead to loss of vision. Depending on the extent of the tear or detachment, these flashes of light might be short-lived or continue indefinitely until the retina is repaired.
You cannot prevent floaters and flashes, but you can prevent vision loss by recognizing the symptoms of retinal tear and retinal detachment. Periodically check the vision in each of your eyes to make sure there are not any new floaters or flashes. Cover one eye and pick a point straight ahead to look at. Count the number of floaters and pay attention to how long and how intense the flashes are. You should see your ophthalmologist if:
- You have never seen floaters and flashes before and all of a sudden you start seeing a lot of them.
- You had floaters and flashes before, but you notice a sudden increase in how many there are.
- A veil or a gray area appears in your peripheral vision or side vision.
- You have had floaters and flashes for a long time, but they now look different than they used to.
- Your floaters interfere with critical tasks such as reading and driving.
- You had floaters in one eye months or years ago and now have them in the other eye.
What is Posterior Vitreous Detachment?
When we age, the vitreous gel thickens and starts to shrink. This causes it to pull away from the retina. The detachment is called posterior vitreous detachment or PVD. Debris from the detachment site drifts into the vitreous and becomes floaters. When PVD happens, a larger sized floater usually develops. This type of floater can look like a cobweb or a veil that blocks part of the vision field. PVD causes the vitreous gel to pull on the retina, producing flashes. When a person is seeing several floaters and flashing lights, it is often a sign of PVD.
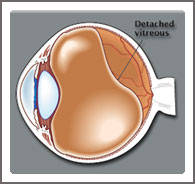
PVD is more likely to occur if a person has had cataract surgery, trauma to the eye or inflammation inside the eye. PVD also occurs more frequently in near-sighted people than in people with normal vision. In most cases, the vitreous will separate cleanly from the retina and will not cause any further problems. The flashes gradually fade away, and then disappear altogether. Floaters caused by PVD may continue, but become less noticeable within two to three months. For some people, the detachment of the vitreous from the retina can cause a tear in the retina. This tear can cause the retina to detach from the back of the eyeball, a serious condition that can cause loss of vision and blindness.
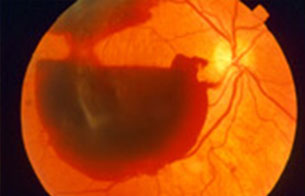
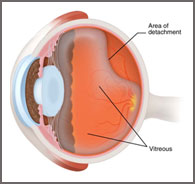
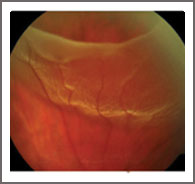
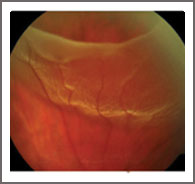
Retinal Detachment
If the vitreous is strongly attached to the retina or if the retina is weak in a certain area, a retinal tear can occur as the vitreous separates from it. Once a retinal tear develops, there is a large chance that the vitreous will go through the tear, causing the retina to detach. This is known as retinal detachment where partial or total loss of vision may occur.
The symptoms of retinal detachment include:
- Sudden increase of floaters
- Flashes of light
- Reduction of vision
- A shadow or curtain in the peripheral vision
What can be done for a retinal break, hole or tear to prevent a retinal detachment?
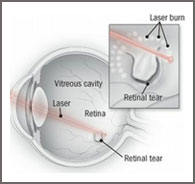
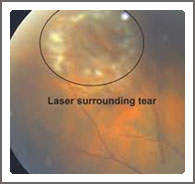
When seen at the correct time, laser treatment can be applied to seal the retina break/hole/tear and help prevent a retinal detachment. When detachment occurs, a procedure called vitrectomy may be performed to repair it. Because of this, it is highly recommended that retinal screening be done at regular intervals: 3, 6 or 12 months depending on the findings seen during screening. Findings may be acceptable now but can change in time.
Is the Retina Screening done for other eye problems?
Yes. Many times patients undergo Retina Screening to explain why vision remains blurred despite the use of eyeglasses. Other times, cataracts alone may not explain why a patient's vision is decreased. An examination of the retina can help make a more accurate assessment of the reason for blurring of vision such as Diabetic Retinopathy and Age-related Macular Degeneration.