Pterygium
- What is a pterygium?
- What are the signs and symptoms associated with pterygium?
- What is the treatment?
Viral Conjunctivitis
- What is viral conjunctivitis?
- What are the signs and symptoms of viral conjunctivitis?
- How do you prevent further transmission?
- Is there a cure for it?
Keratoconus
- What is keratoconus?
- What causes keratoconus?
- What are the signs and symptoms?
- What are the tests used to diagnose keratoconus?
- What is the usual management?
Dry Eye Syndrome
- What is dry eye syndrome?
- What are the symptoms of dry eye?
- What are the treatment options for dry eye?
Contact Lenses
- What are the types of contact lenses?
- How do you care for contact lenses?
- When do you need to visit your eye doctor?
What is a pterygium?
It is a triangular-shaped fleshy tissue that encroaches onto the cornea usually on the nasal (nose) side of the eye. It is thought to be due to environmental factors such as ultraviolet light, chronic dryness and exposure to wind and dust.

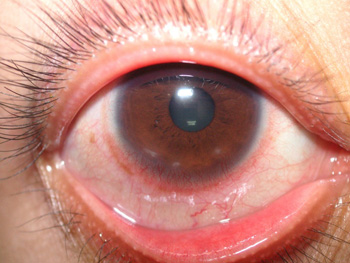
What are the signs and symptoms associated with pterygium?
Patients usually report on and off redness, mild discomfort, feeling of dryness or foreign body sensation and occasional tearing. Blurring of vision may be present if the pterygium encroaches too much onto the cornea causing astigmatism or if it covers the pupil.
What is the treatment?
Surgical excision is indicated if the pterygium progresses towards the center of the cornea or for cosmetic reasons. We perform two types of surgery:
What is viral conjunctivitis?
Viral conjunctivitis or "sore eyes" is usually caused by a virus that can also cause the common cold. It is highly contagious and is spread by hand-to-eye transmission, usually upon touching objects that have come into contact with the infected person's eye secretions or tears.

What are the signs and symptoms of viral conjunctivitis?
The most common symptoms of viral conjunctivitis include redness, tearing, and a burning, sandy, or gritty feeling in one eye. The second eye usually becomes infected within 24 to 48 hours.
How do you prevent further transmission?
Proper hygiene and strict hand washing can help prevent the spread of the infection. It is better to use tissue instead of handkerchiefs to wipe the eye and to dispose of them immediately. Younger children, who may not remember to wash their hands or avoid touching their eyes, should probably not attend school until the discharge has resolved. Older children or adults may choose to attend school/work, but they should limit close contact with others.
Is there a cure for it?
There is no cure for viral conjunctivitis. It is self-limiting, usually lasting 7-10 days, but with some amount of variability depending on the viral strain. Recovery begins after several days, although the symptoms frequently will become worse for the first three to five days followed by gradual improvement over the following one to two weeks.
Treatment is aimed at reducing discomfort, as there is no definitive medication against the viral infection. Cold compresses and artificial tears are used for symptomatic relief. Using breastmilk and urine on the eye are common myths that should be avoided because these may cause secondary bacterial infection (e.g. Gonorrhea, Chlamydia).
Patients should avoid self-medication with over-the-counter eye drops particularly those with steroids, which can cause complications such as glaucoma if used without medical supervision. Patients are strongly advised to consult an ophthalmologist for proper diagnosis and treatment.
What is keratoconus?
This is a fairly common disorder in which the cornea progressively becomes thinner and assumes an irregular cone shape. The condition starts during the adolescent years and progresses slowly over time; after which (around middle age), it may become stationary already. Almost all cases are bilateral, but one eye is usually much more severely affected.
What causes keratoconus?
Etiology is unknown and most likely multifactorial. There seems to be a familial predisposition.
What are the signs and symptoms?
Patients usually note progressive blurring of vision as their astigmatism and myopia increases. Some may report the need to change their glasses or contact lenses frequently.
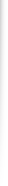
Early signs are only noted by the ophthalmologist using a slitlamp biomicroscope and by corneal topography.
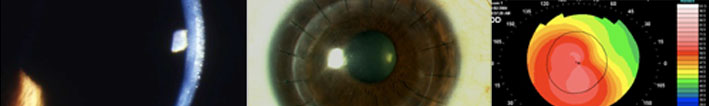
Advanced signs include Munson's signs (bulging of the lower lid when the patient looks down), corneal scarring (opacity).
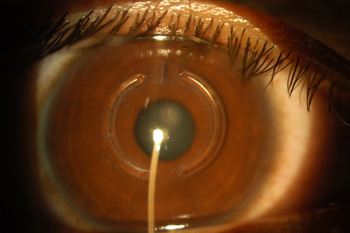
Munson's Signs

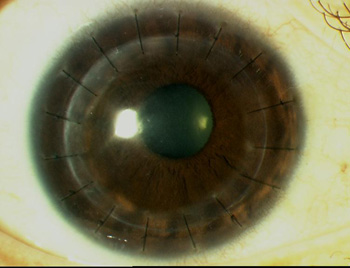
Keratoconus with corneal scarring
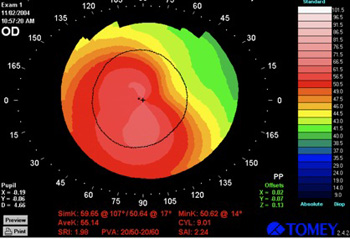
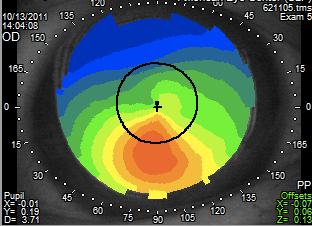
Corneal topography shows steepening of the lower segment of the cornea
What is the usual management?
For mild cases, glasses and toric soft contact lenses may be sufficient in correcting the astigmatism and myopia.
For more advanced cases, rigid gas permeable lenses may prescribed because they help neutralize the irregular astigmatism.
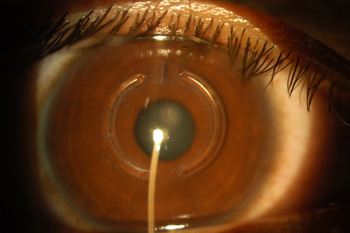
Intrastromal ring segments such as Keraring or Intacs are small, semi-circular plastic implants placed in the middle of the cornea in order to flatten the center and to make its shape more regular.
Collagen Cross-Linking with riboflavin drops is performed by exposing the eye to UV light after instilling riboflavin drops. This strengthens the cornea and stops the progression of keratoconus by creating chemical bonds in between the cornea's collagen fibrils.
Deep anterior lamellar keratoplasty (DALK) is a form of corneal transplantation in which only the anterior/ front layers of the cornea (epithelium until Descemet's membrane) is transplanted. The endothelium of the patient is retained.
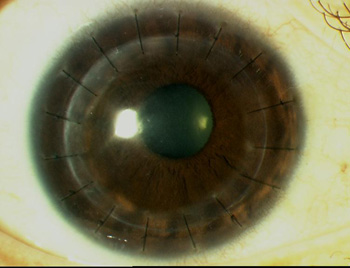
Penetrating keratoplasty is usually the procedure of last resort. The whole cornea including endothelium is transplanted to the patient's eye.
What is dry eye syndrome?
Dry eye is a condition that occurs when there is insufficient production of tears or when tears evaporate too quickly. Tears keep the eye moist and are essential for clear vision. The condition is commonly seen in the elderly (especially in women) but can also occur at any age. Dry eye is associated with immune disorders such as rheumatoid arthritis, eyelid infections and allergies. It can occur in patients taking medications such as antihistamines, nasal decongestants and antidepressants. Infrequent blinking during prolonged computer use can also cause dry eye symptoms.
What are the symptoms of dry eye?
The common symptoms of dry eye include sandy or gritty feeling (foreign body sensation), burning or stinging, pain, redness, excessive tearing, blurring of vision, heavy eyelids and a sticky discharge. Dry eye causes discomfort when using contact lenses and decreased tolerance for reading or using the computer.
What are the treatment options for dry eye?
The first line of therapy for dry eye is the use of artificial tears or gels. They help lubricate the eye and replace the natural tears. Avoid direct wind contact and wear protective glasses when outdoors. Allow your eyes to rest when reading or working on the computer for prolonged periods of time.
Any underlying cause of dry eye needs to be treated. Medications that are prescribed include anti-inflammatory drops (corticosteroids or cyclosporine). In some patients, supplements containing omega-3 fatty acids may help relieve the symptoms. Another option is the use of punctal plugs inserted in the drainage holes of the eyelid, which will block the drainage of tears from the eye to the nose.
What are the types of contact lenses?
There are two main types of contact lenses: rigid gas permeable and soft contact lenses. Rigid gas permeable lenses are made of hard plastic that allows oxygen to pass through and are more durable. Soft lenses are made of thin flexible materials, which absorb water and are more comfortable than rigid lenses. They are available as daily wear, extended wear or disposable lenses.
How do you care for contact lenses?
When do you need to visit your eye doctor?
Remove lenses and consult your eye doctor when you experience acute loss of vision, acute pain and unusual redness, swelling, persistent tearing and persistent blurred vision. Contact lens wearers may be at risk of developing infectious and non-infectious eye problems. Common non-infectious conditions include giant papillary conjunctivitis, sterile corneal infiltrates and corneal warpage.
Infectious keratitis (corneal ulcer) is infection of the cornea, which is a potentially devastating contact lens complication. Early detection is essential to successful treatment.

It is a triangular-shaped fleshy tissue that encroaches onto the cornea usually on the nasal (nose) side of the eye. It is thought to be due to environmental factors such as ultraviolet light, chronic dryness and exposure to wind and dust.

What are the signs and symptoms associated with pterygium?
Patients usually report on and off redness, mild discomfort, feeling of dryness or foreign body sensation and occasional tearing. Blurring of vision may be present if the pterygium encroaches too much onto the cornea causing astigmatism or if it covers the pupil.
What is the treatment?
Surgical excision is indicated if the pterygium progresses towards the center of the cornea or for cosmetic reasons. We perform two types of surgery:
- pterygium excision with mitomycin-C
- pterygium excision with conjunctival grafting.
What is viral conjunctivitis?
Viral conjunctivitis or "sore eyes" is usually caused by a virus that can also cause the common cold. It is highly contagious and is spread by hand-to-eye transmission, usually upon touching objects that have come into contact with the infected person's eye secretions or tears.

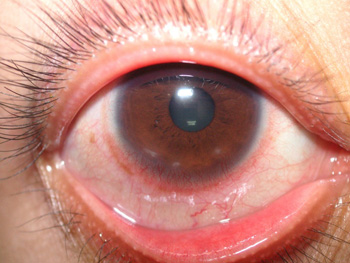
What are the signs and symptoms of viral conjunctivitis?
The most common symptoms of viral conjunctivitis include redness, tearing, and a burning, sandy, or gritty feeling in one eye. The second eye usually becomes infected within 24 to 48 hours.
How do you prevent further transmission?
Proper hygiene and strict hand washing can help prevent the spread of the infection. It is better to use tissue instead of handkerchiefs to wipe the eye and to dispose of them immediately. Younger children, who may not remember to wash their hands or avoid touching their eyes, should probably not attend school until the discharge has resolved. Older children or adults may choose to attend school/work, but they should limit close contact with others.
Is there a cure for it?
There is no cure for viral conjunctivitis. It is self-limiting, usually lasting 7-10 days, but with some amount of variability depending on the viral strain. Recovery begins after several days, although the symptoms frequently will become worse for the first three to five days followed by gradual improvement over the following one to two weeks.
Treatment is aimed at reducing discomfort, as there is no definitive medication against the viral infection. Cold compresses and artificial tears are used for symptomatic relief. Using breastmilk and urine on the eye are common myths that should be avoided because these may cause secondary bacterial infection (e.g. Gonorrhea, Chlamydia).
Patients should avoid self-medication with over-the-counter eye drops particularly those with steroids, which can cause complications such as glaucoma if used without medical supervision. Patients are strongly advised to consult an ophthalmologist for proper diagnosis and treatment.
What is keratoconus?
This is a fairly common disorder in which the cornea progressively becomes thinner and assumes an irregular cone shape. The condition starts during the adolescent years and progresses slowly over time; after which (around middle age), it may become stationary already. Almost all cases are bilateral, but one eye is usually much more severely affected.
What causes keratoconus?
Etiology is unknown and most likely multifactorial. There seems to be a familial predisposition.
What are the signs and symptoms?
Patients usually note progressive blurring of vision as their astigmatism and myopia increases. Some may report the need to change their glasses or contact lenses frequently.
Early signs are only noted by the ophthalmologist using a slitlamp biomicroscope and by corneal topography.
Advanced signs include Munson's signs (bulging of the lower lid when the patient looks down), corneal scarring (opacity).
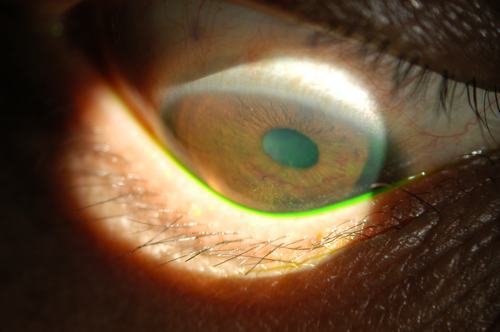
Munson's Signs

Keratoconus with corneal scarring
What are the tests used to diagnose keratoconus?
Corneal topography creates a color map of the corneal surface using Placido rings, which shows the steep and flat areas of the cornea. In patients with keratoconus, the lower part of the cornea is significantly steeper than the upper part.
Pachymetry measures the thickness of the cornea especially in the center. The cornea is thinner in keratoconus compared to the normal population.
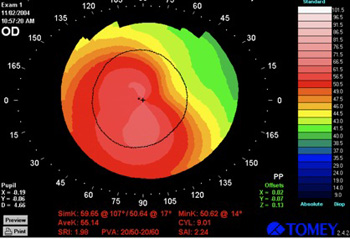
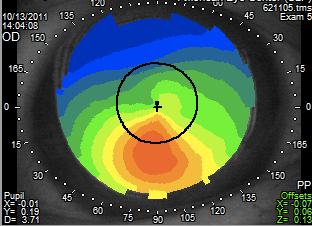
Corneal topography shows steepening of the lower segment of the cornea
What is the usual management?
For mild cases, glasses and toric soft contact lenses may be sufficient in correcting the astigmatism and myopia.
For more advanced cases, rigid gas permeable lenses may prescribed because they help neutralize the irregular astigmatism.
Intrastromal ring segments such as Keraring or Intacs are small, semi-circular plastic implants placed in the middle of the cornea in order to flatten the center and to make its shape more regular.
Collagen Cross-Linking with riboflavin drops is performed by exposing the eye to UV light after instilling riboflavin drops. This strengthens the cornea and stops the progression of keratoconus by creating chemical bonds in between the cornea's collagen fibrils.
Deep anterior lamellar keratoplasty (DALK) is a form of corneal transplantation in which only the anterior/ front layers of the cornea (epithelium until Descemet's membrane) is transplanted. The endothelium of the patient is retained.
Penetrating keratoplasty is usually the procedure of last resort. The whole cornea including endothelium is transplanted to the patient's eye.
What is dry eye syndrome?
Dry eye is a condition that occurs when there is insufficient production of tears or when tears evaporate too quickly. Tears keep the eye moist and are essential for clear vision. The condition is commonly seen in the elderly (especially in women) but can also occur at any age. Dry eye is associated with immune disorders such as rheumatoid arthritis, eyelid infections and allergies. It can occur in patients taking medications such as antihistamines, nasal decongestants and antidepressants. Infrequent blinking during prolonged computer use can also cause dry eye symptoms.
What are the symptoms of dry eye?
The common symptoms of dry eye include sandy or gritty feeling (foreign body sensation), burning or stinging, pain, redness, excessive tearing, blurring of vision, heavy eyelids and a sticky discharge. Dry eye causes discomfort when using contact lenses and decreased tolerance for reading or using the computer.
What are the treatment options for dry eye?
The first line of therapy for dry eye is the use of artificial tears or gels. They help lubricate the eye and replace the natural tears. Avoid direct wind contact and wear protective glasses when outdoors. Allow your eyes to rest when reading or working on the computer for prolonged periods of time.
Any underlying cause of dry eye needs to be treated. Medications that are prescribed include anti-inflammatory drops (corticosteroids or cyclosporine). In some patients, supplements containing omega-3 fatty acids may help relieve the symptoms. Another option is the use of punctal plugs inserted in the drainage holes of the eyelid, which will block the drainage of tears from the eye to the nose.
What are the types of contact lenses?
There are two main types of contact lenses: rigid gas permeable and soft contact lenses. Rigid gas permeable lenses are made of hard plastic that allows oxygen to pass through and are more durable. Soft lenses are made of thin flexible materials, which absorb water and are more comfortable than rigid lenses. They are available as daily wear, extended wear or disposable lenses.
How do you care for contact lenses?
- Always wash hands with soap and water and dry hands before handling lenses.
- Learn the proper technique of inserting and removing lenses.
- Clean and disinfect lenses daily and store properly.
- Use solutions recommended by your doctor.
- Don't use tap water or saliva to wet lenses.
- Don't wear damaged lenses.
- Don't sleep with lenses.
- Never wear another person's contact lenses.
- Keep a pair of glasses as back-up.
- Buy contact lenses from reputable optical shops or eye clinics.
When do you need to visit your eye doctor?
Remove lenses and consult your eye doctor when you experience acute loss of vision, acute pain and unusual redness, swelling, persistent tearing and persistent blurred vision. Contact lens wearers may be at risk of developing infectious and non-infectious eye problems. Common non-infectious conditions include giant papillary conjunctivitis, sterile corneal infiltrates and corneal warpage.
Infectious keratitis (corneal ulcer) is infection of the cornea, which is a potentially devastating contact lens complication. Early detection is essential to successful treatment.